| Cardiology Patient Education Series |
The following topics will walk you through the basics and more of your specific condition and the treatments available. You will find helpful pictures, videos and information on common heart problems. Each topic will provide background information as well as common diagnostics tests and treatments. |
| Diseases: |
|
| |
| Heart Basics |
| The heart has 4 chambers: 2 atria and 2 ventricles. They are all separated but have specific openings for blood to flow through them. Blood returns from the body to the right atrium to the right ventricle to the lungs to the left atrium to the left ventricle and to the aorta and body. The tissue that separates the right and left atria and ventricles is called a septum |
 |
| |
Video Explaining basic heart function and common problems:
https://www.youtube.com/watch?v=H04d3rJCLCE |
|
| Common Heart Tests |
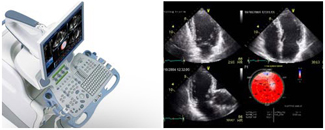
Echocardiogram (Echo) |
 |
|
| An Echo is an ultrasound of the heart. This is a very important test that gives a lot of information about the heart structure and function. It is a safe test that can be done easily in the Doctor’s office. A machine with a special probe is used to generate pictures. There are different kinds of echocardiograms: |
- Transthoracic (TTE) – the probe is placed on the chest for acquisition of ultrasound images of the heart. This test provides information for the pumping function of the heart as well as narrowing or leakage of heart valves. The test takes 30-60 minutes and no preparation is required.
- Transesophageal (TEE) – the probe is inserted through the mouth and down the esophagus into the stomach. The test is requested when more detail for the heart valves or pumping function is required than available by transthoracic echocardiogram. The test takes 30-60 minutes and done on an empty stomach with 8-10 hour fasting. Patient receives a sedative medication to avoid discomfort but remains awake during the test.
- Stress Echo – a special transthoracic echocardiogram when ultrasound images of the heart are obtained immediately after exercise (treadmill or supine bicycle) or after administration of a medication that makes the heart work harder than normal to assesses heart function under stress. The test takes 60-90 minutes and no special preparation is required.
|
|
Electrocardiogram (ECG or EKG) |
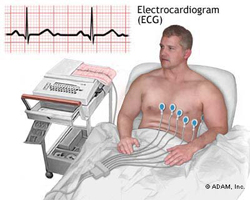 |
An ECG is an electrical exam of the heart. Several electrodes are placed strategically around the chest and connected to a machine that converts the electrical information into a series of line tracings that can be interpreted by a Physician. This is a very quick and safe test that gives a lot of information about the health of the heart. This is often one of the first tests done when you see a heart specialist. |
|
| Cardiac Catheterization |
| This is a test when a catheter is advanced from the artery in the wrist or groin area into the heart for pressure measurement inside the chambers of the heart and dye injected to detect any blockages that may be obstructing adequate blood flow to the heart muscle. If present, these blockages may be treated with placement of a stent (small tubes made of stainless steel mesh) or require open heart surgery when the blockages can be bypassed using a vein from the leg. |
| https://www.youtube.com/watch?v=pWfGjNeUyo8 |
| Coronary Stenting |
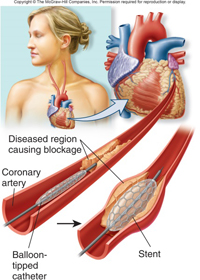 |
This is a procedure that treats blockages in the heart vessels. It involves inserting a device that will clear the blockage and relieve symptoms of chest pain and shortness of breath. It consists of angioplasty (opening up of the vessel) and stent placement. This procedure requires the patient to be under sedation and pain medications. An interventional Cardiologist performs this procedure in a catheter lab (much like an Operating Room). After sedation, a local anesthetic is used to numb the groin area before inserting the needle. A guide wire is inserted in the vein first and is easily advanced up to the area of blockage outside the heart. Next, a balloon catheter which is a small flexible tube with an inflatable tip is inserted over the guide wire and advanced to the location of the blockage. Once in place, the balloon with the stent is inflated opening it up and restoring patency to the vessel. The catheter is removed and the stent remains in place. Angiography (radiographic imaging of the vessels using specific dye) can be used before during and after the procedure to help the cardiologist visualize the blockage and vessels better. |
 |
There are 2 types of stents: a bare metal stent and drug-eluting stent. The bare metal stent is made of stainless steel or cobalt-chromium steels and has slots that make it expandable. The drug-eluting stent is a metal stent that is laced with a drug that is steadily released from the stent weeks. This drug helps prevent that area from closing up again (restenosis). Because of this added benefit the drug-eluting stent is used more commonly.
Coronary stenting is a same-day procedure that takes from 30 minutes to 3 hours and is a very safe. Before the procedure you will need to fast for 8-10 hours. After the procedure the Physician will prescribe some medications to help prevent further blockages. |
|
| Chest Pain Assessment |
Chest pain is one of the most distressing symptoms for many people because it can represent a heart attack. But there are many different causes for chest pain. Physicians have different tools available to come up with the causes of chest pain. The first thing that must be done is a quick history to get a good description of the chest pain. The next step is an EKG because it is a quick test that shows changes in electrophysiology of the heart. If the EKG shows some areas of ischemia (blockage) lab tests will be ordered, medications are started and cardiac catheterization is scheduled. If heart attack can be ruled out then other causes of chest pain can be explored. For more information on heart attacks see below.
Some other causes of chest pain include: GERD (gastroesophageal reflux disease or heartburn), angina, pericarditis, costochondritis, pulmonary embolism and arrhythmias. Further questioning, physical exams, vital signs, lab tests, radiologic tests might be needed to differentiate what the specific cause of the chest pain is. Chest pain is always taken seriously. |
 |
|
| Heart Attack a.k.a. Myocardial Infarction (MI) |
| What is that? |
 |
A heart attack occurs when there is death of cardiac (heart) tissue due to lack of blood supply to that portion. This is a result of coronary artery disease. Even though CAD develops slowly over time a heart attack can happen suddenly and cause significant damage. This is because a clot from a plaque in the blood vessels can break off and travel down to smaller arteries around the heart, get stuck and block blood from getting by. The tissue beyond the blockage is left without any blood supply and dies very quickly. This is very dangerous because this can cause serious arrhythmias and pumping problems that can lead to death. |
| Recognition of symptoms is very important. Use of nitroglycerin at this point might be helpful. The most important thing to do is call for medical help (911). Once under medical care an EKG may confirm whether a heart attack exists and if so the type of heart attack and which area is involved. The Physician will then put together all the evidence and decide on the next appropriate step. |
| Symptoms |
| Severe chest pain and at times left arm pain, shortness of breath, heart racing, sweating, nausea and anxiety can all occur during a heart attack. Some populations such as diabetics, women or elderly may not have these typical symptoms. |
| Treatment |
| Pain medications are given to relieve the pain. Oxygen might be given if there is difficulty breathing and oxygen levels are decreased. Nitroglycerin may or may not help relieve the symptoms, aspirin is also given. If the patient arrives early enough thrombolytic medication (clot busters) can be given to get rid of the clot. A non-invasive procedure, coronary stenting is usually done to reopen the blocked area in the artery using a catheter. Further surgical procedures may be needed. |
| It is very important to be aware of the symptoms and immediately seek medical attention. Certain treatments can only be administered if you make it to the hospital within 90 minutes. |
|
| Palpitations / Arrhythmias |
| What is that? |
| A palpitation is an awareness of one’s heart beating. It could represent an abnormal or normal heart rhythm. It is often associated with a premature beat. Because it could represent a serious cardiac condition it has to be further investigated with tests. |
| An arrhythmia is an abnormal heart rhythm. The heart’s pumping function is controlled through an electrical conduction system. The pacemaker is the sinoatrial node in the wall of the right atrium. From this node, signals are sent to both atria and ventricles in distinct pathways within the heart wall that tell the heart contract. When this conduction system is not functioning there will be an abnormal rhythm. There are several different types of abnormal rhythms with different patterns. Each type represents a different condition and must be investigated. An EKG shows the pattern of the rhythm. They can represent anxiety, heart blocks, nerve disorders, alternate conduction pathways. They can be associated with congenital heart diseases, cancers, heart failure. Some common arrhythmias are atrial fibrillation, atrial flutter, premature ventricular contractions, ventricular tachycardia, |
| Treatments depend on the specific type of arrhythmia. |
| Coronary Artery Disease (CAD) |
| What is that? |
| Coronary artery disease is the leading cause of death in USA, Europe and #2 in Canada. It is damage to the arteries of the heart. This is also called atherosclerosis, the buildup of plaque in the arteries. This buildup of plaque in the arteries narrows the arteries and can lead to blockages in different areas. When it blocks arteries in the heart muscle it causes heart attack. When it blocks arteries in the brain it causes stroke. The plaque builds up slowly over several years and may not cause any symptoms or damage until a heart attack or stroke occurs. Some signs and symptoms might include chest pain, palpitations, fainting, exercise intolerance, or blurry vision. |
| Family history is also an important factor in determining who gets it. Risk factors for developing coronary artery disease include high cholesterol, smoking, hypertension, diabetes and psychosocial stress. A balanced diet and exercise can help prevent coronary artery disease or delay its progression. |
| Special Populations: South Asian Community |
| Studies show that South Asians have a 3-5 fold increase in risk for heart attack and cardiovascular disease compared to other ethnic groups. |
| South Asians are also more likely to get coronary artery disease at a younger age, often before 40 and have more severe disease. They also have high mortality rates compared to other groups. |
| This finding might be explained by both genetic predisposition and environmental influences. This population also has one of the highest rates of diabetes mellitus. South Asians have increased abdominal obesity which increases insulin resistance and even when BMI is normal increases their chances of getting diabetes. |
| (Data from article: South Asians and Cardiovascular Risk) |
| Studies show that South Asians have a 3-5 fold increase in risk for heart attack and cardiovascular disease compared to other ethnic groups. |
| South Asians are also more likely to get coronary artery disease at a younger age, often before 40 and have more severe disease. They also have high mortality rates compared to other groups. |
| This finding might be explained by both genetic predisposition and environmental influences. This population also has one of the highest rates of diabetes mellitus. South Asians have increased abdominal obesity which increases insulin resistance and even when BMI is normal increases their chances of getting diabetes. |
|
| (Data from article: South Asians and Cardiovascular Risk) |
| Screening |
| Coronary artery disease is so common and in some cases preventable as long as proper steps are taken. The first step is to assess individual risk factors to see if there is a great chance of developing CAD. Based on these risk factors you might fall in one of the following categories: low risk, intermediate risk or high risk. The next step is to address the modifiable risk factors such as hypertension, high cholesterol, smoking and diabetes. Preventing CAD involves properly treating these diseases. If you are in the intermediate or high risk category further screening tests such as EKG, treadmill stress test, blood tests, urine tests and blood pressure monitoring may be ordered. Some of these screening tests will need to be redone periodically to monitor your progress. To prevent getting or delay progression of CAD requires proper nutrition, exercise and regular visits with your Physician. |
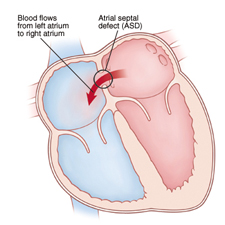
| Atrial Septal Defect (ASD) |
| What is it? |
ASD is a heart condition that represents an abnormal communication (hole) in the upper chambers of the heart. Commonly, this hole closes early in life but rarely it might remain open. If this hole persists it will slowly overwork the heart over the years. This is why it needs to be identified and surgically closed. If uncorrected, the heart will become enlarged and patient will develop heart failure.
The ASD changes how the heart normally functions because it affects the normal pressures and volumes in the heart. When there is an ASD, blood leaks through the hole, from left to right, with each pumping action of the heart. The right side has to handle more blood and will grow bigger to try to handle the extra blood but eventually become weak. These processes take time, so it is possible for a patient to have no symptoms until adulthood. Some of the symptoms include shortness of breath, fatigue, palpitations or heart failure. To prevent any permanent damage to the heart, cardiologists prefer to close the ASD early in life.
ASDs are classified into three types (Ostium primum, Ostium secundum, and Sinus venosus) depending on the location of the defect within the inter-atrial septum. Ostium secundum is the most common type. |
 |
| How is it diagnosed |
- 2 dimensional(2D) Echocardiogram with color flow mapping confirms diagnosis
- EKG
|
|
| How is it treated? |
Most Secundum ASD can be treated by a catheter approach without the need for open heart surgery. A catheter is advanced to the heart from the vein in the groin and placed across the defect. Using X-Ray and ultrasound guidance, a double umbrella device is implanted through the catheter, capturing the hole between the two discs of the umbrella device. The device remains in the heart and scar tissue forms over the umbrella device over time and permanently seals the hole. A successful procedure will resolve patient |
 |
|
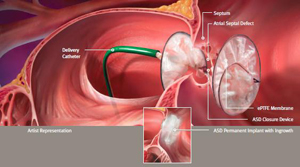 |
symptoms related to ASD and prevent any worsening of the heart function in the future. Closure of ASD done at an early age provides greater long term benefit compared to that done in later part of life. This procedure is done in the operating room under anesthesia and usually only requires overnight hospital stay. Recovery is also quick.
http://www.youtube.com/watch?v=I5sRAcOVGiU |
| After the procedure you may have some minor pain at the incision site and will have a bandage for 4-6 weeks. Normal activity can resume after 2 days but vigorous activity should be limited for 2 weeks. The Physician will also prescribe some medications to prevent blood from clotting. |
|
|
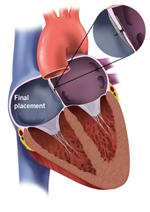
| Patent Foramen Ovale (PFO) |
| What is it? |
| Before birth there is a natural opening in the atrial septum that allows blood to flow from right atrium to left atrium called the foramen ovale. After birth this opening normally closes. But in some infants this opening remains open and blood continues to flow between the atria, a patent foramen ovale. This opening causes changes in the heart that over time can lead to heart failure. Patient can experience symptoms such as headaches, dizziness or shortness of breath. This opening can also predispose patients to strokes because a blood clot can travel from veins to the right side of the heart through the PFO bypassing the lungs to the left side of the heart and to the head, causing a stroke. A characteristic of PFO’s is strokes at a young age. Surgical closure of PFO protects against these strokes. |
 |
|
| What is it? |
- Echocardiogram with color flow mapping confirms diagnosis
- ECG
- Cardiac catheterization – sometimes this is done to see how healthy the lungs are
|
|
| What is the treatment? |
- Medications (blood thinners) can be given to help prevent clots from causing strokes.
- Transcatheter closure of the PFO is done for patients that have had complications like strokes while on other therapies. A catheter with a special tip is inserted through a needle into the femoral vein in the groin area and advanced to the heart. The catheter tip contains two circular meshes that are deployed on either side of the opening. Special imaging techniques are used to visualize and ensure correct placement of the mesh. The catheter is removed leaving a permanent closure of the PFO. Once the opening is closed there is decreased risk for future strokes. This procedure has great success and takes only 1-2 hours.
|
 |
PFO closure animation video: http://www.youtube.com/watch?v=ZOtk_FSfHpw |
| Ventricular Septal Defect (VSD) |
| What is it? |
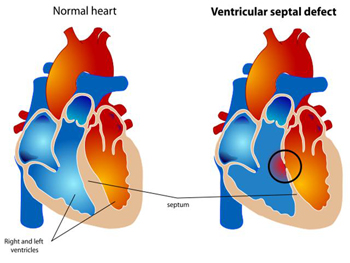 |
A VSD is condition caused by a defect (a hole) in the ventricular septum that separates the left and right ventricles. This causes an unnatural exchange of blood through the hole. This is the most common defect found at birth. Oftentimes the VSD will close spontaneously in childhood but other times it remains open and causes severe symptoms in adulthood. Severity of symptoms depends on the severity of the defect and the health of the heart and lungs. Some of these include shortness of breath, chest pain, fainting, blue toes and fingers, clubbing (thickening of nails) or thickening of the blood. |
| Most of these symptoms will not be present at the same time. |
|
| VSDs are classified based on the part of the septum the defect is located: membranous, peri-membranous, and muscular. VSDs may be associated with other abnormalities such as Down syndrome, DiGeorge syndrome, Turner syndrome and Tetralogy of Fallot. |
|
| How is it diagnosed? |
- Echocardiogram
- ECG – Shows signs of a large right ventricle
- Cardiac catheterization – shows the extent of damage to blood vessels in the lungs
|
|
|
| How is it treated? |
| Medical treatment includes heart failure medications such as diuretics, digoxin and ACE inhibitors. These medications can improve heart pumping function and decrease symptoms. They might work well for a while but ultimately medium to large VSDs will need to be closed to prevent permanent damage to the heart and lungs. |
|
| Surgery is needed when heart failure progresses and lung dysfunction occurs. There are 2 surgical options used to close the defect: open heart or transcatheter closure. The open heart approach is much more involved and must be done under anesthesia. The chest is opened, then the heart is stopped using either ice or medications. The blood pumping and oxygenation functions are taken over by a cardiopulmonary bypass machine (heart-lung machine). The surgeons then open up the heart to locate the defect and sew a patch over it. After the defect is closed the bypass machine is turned off and blood returns to the heart. A small chest tube is placed to drain excess fluids and the chest is closed. This operation takes 2-4 hours. The patient might spend around 4 days in hospital before being discharged home. This is a major surgery with some possible complications and is thus only recommended to patients that are in good enough health to undergo this operation. |
|
| An alternative to open heart surgery is the transcatheter approach. This procedure does not require the opening the heart as it is a minimally invasive procedure. This makes it an ideal option for elderly patients who could not undergo open heart surgery. A needle is inserted through the skin into a vein in the femoral (groin) area and advanced to the heart ventricles where the defect exists. Then a special mesh at the tip of the catheter is inserted between the holes closing it up. Special imaging allows the cardiologist to visualize what is happening and make sure it is correctly placed. The procedure takes about 1-2 hours and patient can go home after 1-3 days. |
|
| Video of a transfemoral VSD closure: http://www.youtube.com/watch?v=QuV1k3I7Apw |
| |
| |
| |
| References |
| -Pictures from Kramesonline.com, (St. Judes) http://health.sjm.com/pfoandstroke-answers/your-treatment/transcatheter-pfo-closure |
|
-Oxford textbook of medicine (2010) |
-Merck Manual of Diagnosis and Therapy (2011) |
-Harrison’s Principles of Internal Medicine 18th Edition (2012) |
| http://healthtravelnetwork.com/(S(50wxl4mxiqe0tuwb4oixnnrf))/treatmentdetails.aspx?tid=7&AspxAutoDetectCookieSupport=1 (VSD picture) |
|
| Congenital Heart Disease for the Adult Cardiologist Ventricular Septal Defects. Mary S. Minette, David J. Sahn |
| American Heart Association - http://watchlearnlive.heart.org/CVML_Player.php?moduleSelect=replac |
| Childrens hospital: http://www.childrenshospital.org/health-topics |
Schwartz’s Principles of Surgery |
| http://www.pted.org/?id=pfo3 |
|
|
|
| |
| |